
Electronic Health Records (EHRs) transform how healthcare providers manage patient information. EHRs offer many advantages, including increased efficiency, better patient outcomes, and improved care coordination.
However, several challenges are associated with EHR adoption, such as issues with data accuracy, data privacy, and physician burnout. As healthcare organizations continue to adopt EHRs, it is essential to understand both the benefits and challenges of this technology.
In this blog, we will explore the pros and cons of EHRs, their impact on patient engagement, challenges related to their adoption, and strategies to address these challenges. By this blog's end, you will better understand EHRs and their potential to transform the healthcare industry.
Let’s look at the pros first before you review the disadvantages that may hamper the implementation of EHR in medical diagnosis.
One of the most significant advantages of electronic health records (EHRs) is improved patient care. EHRs enable healthcare providers to access real-time patient information, including medical history, test results, and medication information. This real-time access allows providers to make informed decisions about patient care, resulting in better outcomes and more personalized treatment plans.
EHRs improve efficiency by reducing administrative tasks, such as charting, filing, and transcription, allowing providers to spend more time with patients. This paperwork reduction also leads to faster turnaround times and less time spent on data entry.
EHRs can help healthcare providers save money by reducing the costs of paper-based systems, such as physical storage and supplies. Additionally, EHRs can help prevent errors and duplicate tests, leading to cost savings over time.
EHRs allow for easier collection and analysis of healthcare data, which can help providers make more informed decisions about patient care. This data can also identify trends and patterns to help providers better understand patient needs and diagnose more accurately.
EHRs enable better communication between healthcare providers, resulting in better care coordination and fewer mistakes. EHRs can also improve communication between patients and providers, allowing patients to access their medical information and communicate with their healthcare team.
EHRs can improve the accuracy of patient information by reducing the potential for human error associated with paper-based systems. EHRs also make it easier for providers to track changes in patient data, resulting in more accurate and up-to-date records.
EHRs enable patients and healthcare providers to access health information anywhere, anytime. This access allows providers to make informed decisions about patient care and enables patients to take a more active role in their healthcare.
EHRs can help improve patient safety by reducing errors and improving the accuracy of patient information. Additionally, EHRs can help prevent adverse drug events by alerting providers to potential drug interactions and allergies.
EHRs can help streamline healthcare providers' workflow by reducing the paperwork and administrative tasks associated with paper-based systems. This streamlined workflow can result in faster turnaround times and increased productivity.
Overall, the use of EHRs can lead to better patient outcomes by improving the accuracy of patient information, enabling better care coordination, and providing more personalized treatment plans.
Despite being so advantageous, EHR has a few drawbacks to consider before choosing the technology.
One of the biggest concerns associated with EHRs is the security of patient information. EHRs can be vulnerable to cyber attacks, and healthcare providers must take steps to ensure that patient data is secure.
EHRs can also raise concerns about patient privacy. Patients may be concerned about who can access their medical information and how it is used.
While EHRs can improve the accuracy of patient information, they are not immune to errors. Technical difficulties and human error can result in inaccurate records, seriously affecting patient care.
While EHRs can improve efficiency in many areas, they can also increase the time required for data entry. Providers must ensure that all information is accurately recorded in the system, which can take time away from patient care.
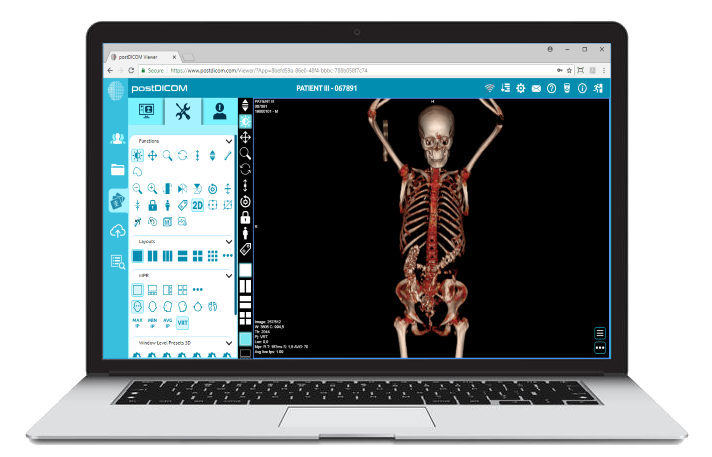
 - Created by PostDICOM.jpg)
EHRs promote patient engagement by providing access to their health information, facilitating communication between patients and providers, and enabling personalized care. EHRs can improve health outcomes and patient satisfaction by engaging patients in their healthcare.
Access to Health Information: EHRs give patients access to their health information, including test results, diagnoses, and treatment plans. This lets patients stay informed about their health and take a more active role in their care.
Communication: Healthcare record automation can facilitate communication between patients and their healthcare providers. Patients can use secure messaging or telehealth platforms to communicate with their providers, ask questions, and receive medical advice.
Preventative Care: EHRs can help providers identify patients due for preventive care, such as vaccinations or cancer screenings. Providers can then reach out to patients and encourage them to schedule appointments, improving health outcomes.
Personalized Care: Record automation can provide providers with a comprehensive view of a patient's health history, informing customized care plans. Providers can use this information to tailor treatments and care plans for each patient's needs.
Health Tracking: The technology can integrate with wearable devices and mobile apps, allowing patients to track their health and wellness goals. Patients can then share this information with their providers, informing treatment plans and leading to improved health outcomes.
Adopting Electronic Health Records (EHRs) can present several challenges for healthcare providers. Here are some of the most common challenges:
EHRs can be expensive to implement and maintain, with costs ranging from tens of thousands to millions of dollars, depending on the size of the healthcare organization.
Healthcare providers must be trained on how to use EHRs effectively, which can be time-consuming and costly. Additionally, healthcare organizations must invest in ongoing training to keep providers up-to-date with the latest software updates and technology advancements.
EHRs from different vendors may not be compatible, making it difficult for providers to share patient information across different systems. This lack of interoperability can result in gaps in patient information and potentially compromise patient care.
Implementing and maintaining EHRs requires technical expertise, which may be lacking in some healthcare organizations. Technical challenges like system crashes or downtime can also disrupt patient care and workflow.
Providers may find the process of entering patient information into an EHR system to be time-consuming and disruptive to workflow. This can result in providers being hesitant to adopt the EHR system fully and instead relying on paper-based systems.
EHRs can be vulnerable to cyber attacks and breaches, compromising patient data privacy and security. Healthcare organizations must ensure that patient data is protected and secure.
The transition from paper-based systems to EHRs can be challenging for some healthcare providers, who may resist change or have concerns about the new system's effectiveness.
Electronic Health Record (EHR) data accuracy is a significant issue healthcare providers face. EHR data is only as accurate as the data entered, and errors can occur for various reasons.
Data Entry Errors: EHR data entry can be prone to errors, such as typos or incorrect codes. For example, a provider may accidentally input the wrong medication dosage, leading to serious patient safety issues.
Duplicate or Overlapping Data: Patients may have duplicate records in the EHR system, resulting in conflicting information or duplicate lab tests. Overlapping data can also occur if providers enter information multiple times, leading to inaccuracies in the patient record.
Lack of Standardization: EHR data is often not standardized, meaning that different providers may input information differently. This can lead to confusion and errors in patient records.
System Integration Issues: EHRs may not integrate seamlessly with other systems, leading to missing or incomplete data. For example, if a lab system does not integrate with an EHR system, lab results may not be automatically uploaded to the patient's record, leading to inaccuracies.
Data Quality Issues: EHR data may be incomplete, inconsistent, or outdated, leading to inaccuracies in patient records. This can result in misdiagnoses or improper treatment plans.
To address these issues, healthcare providers must ensure that EHR data is accurate and up-to-date. This may involve implementing standardized data entry processes, training staff on proper data entry techniques, and conducting regular audits of patient records to identify and correct errors.
Electronic Health Records (EHRs) have been linked to physician burnout, a significant problem in the healthcare industry. Burnout can lead to decreased job satisfaction, increased medical errors, and reduced patient outcomes.
EHRs can be time-consuming, requiring physicians to document patient information more. This can lead to a higher workload, which can contribute to burnout.
The system may disrupt physician workflows, leading to frustration and inefficiency. For example, physicians may have to navigate multiple screens or tabs to find the necessary information, which can be stressful.
Typically, EHRs can generate large amounts of data, which can be overwhelming for physicians to manage. Physicians may feel pressure to review all the available data, leading to burnout and cognitive overload.
Sometimes the system can interfere with the doctor-patient relationship. Physicians may feel pressure to document everything during the visit, leading to less time for personal patient interactions.
EHR systems can vary widely in design and functionality, leading to frustration and inefficiencies for physicians who must navigate multiple systems.
Electronic Health Records (EHRs) offer many advantages for healthcare providers and patients. EHRs can improve efficiency, reduce medical errors, and provide better access to patient information.
However, several challenges are associated with EHR adoption, including data accuracy, data privacy, and physician burnout. Healthcare providers must address these challenges to maximize the benefits of EHRs while minimizing the risks.
By implementing best practices for EHR adoption, healthcare providers can improve patient outcomes, reduce costs, and enhance the overall quality of care. As the healthcare industry continues to evolve, EHRs will undoubtedly play a critical role in shaping the future of healthcare delivery.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |