 - Created by PostDICOM.jpg)
When you hear the term ‘medical imaging’, the first picture that comes to mind is that of a radiograph, or an X-ray as it is more commonly known. While radiographs are the oldest and still the most frequently employed method of medical imaging, there is so much more to this intriguing and innovative field of science today. In this article, we attempt to review the current state of affairs and latest advancements in medical imaging technology as well as delineate areas where major breakthroughs are anticipated in the not-too-distant future.
The term ‘medical imaging technology’ has a broad definition and encompasses any technique that helps medical professionals view the interior of the body or areas that are not visible to the naked eye. Visualization of these structures can aid in the diagnosis of disease, treatment planning, treatment execution—such as through image-guided intervention, and monitoring and surveillance.
 - Created by PostDICOM.jpg)
Today, medical imaging is integral to disease diagnosis and management. The earliest form of diagnostic medical imaging was the X-ray unit, introduced by Roentgen in 1895. Since then, radiographic imaging has come a long way, and traditional X-rays are being replaced rapidly by computed tomography (CT), which combines the power of computer processing with X-ray imaging. CT scanners take images in three different planes. CT technology itself has undergone refinement over the years. The thickness of image slices has been reduced and the spiral CT has arrived which dramatically reduces image acquisition time.
Magnetic resonance imaging (MRI) emerged at the end of the twentieth century, at a time when concerns about radiation exposure during medical imaging were at a peak. This imaging system uses natural magnetic fields to acquire images of internal body structures. Although initially the MRI had limited diagnostic use, improvements in the equipment have allowed it to become the imaging modality of choice for soft tissues and vascular structures. Newer MRI machines are compact and open devices that no longer make patients feel claustrophobic.
Ultrasonography is another imaging modality that does not employ radiation. It uses reflected sound waves to paint a picture of internal organs. A major advantage of ultrasound is its portability. It has gained widespread medical application such for bedside examinations, studying vascular structures, and in obstetrics for assessing fetal health.
Other advanced medical imaging techniques have harnessed the power of nuclear radioisotopes. Positron emission tomography (PET) allows radiolabeled molecules, such as glucose, to be taken up by body tissues. They are then detected by sensors and their distribution gives clues to the diagnosis. The introduction of contrast media has led to site-specific imaging such as CT angiography. Radiolabeled material is injected into the bloodstream and vascular structures can be easily visualized. This helps in identifying vascular anomalies and bleeders. Radiolabeled molecules can also be taken up by certain tissues, which helps in narrowing down a diagnosis. For instance, technetium-99 is used in bone scanning and iodine-131 is used to study thyroid tissue. Often two or more of the above imaging techniques are combined to give the physician a definite idea of what is going on in the patient’s body.
Medical imaging technology has progressed by leaps and bounds over the years. This hasn’t been limited to the modalities through which images are acquired. There has been an ever-increasing emphasis on postprocessing and newer more advanced ways of sharing and storing medical images. The idea here is to extract the maximum benefit out of existing technologies and spread it to the most number of people possible.
In the realm of diagnostic medical imaging, clinicians can now manipulate images to gain greater insights and information from the same set of data.
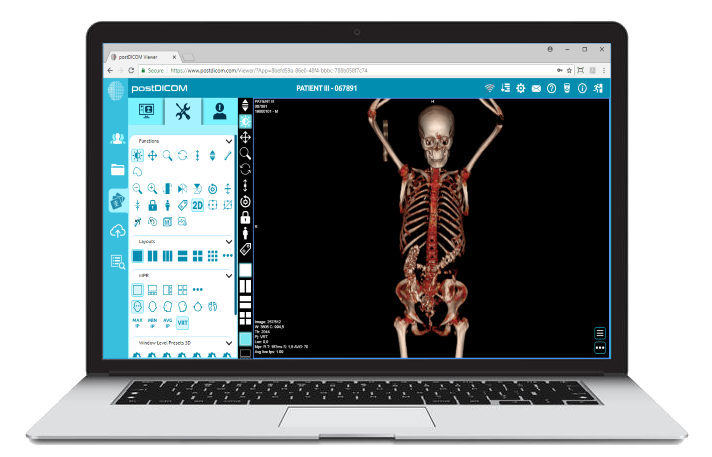
With the different types of imaging devices employed today and the unique data that they produce, integration and ease of collaboration are of paramount interest to healthcare institutes and end users. Almost all types of images today are acquired digitally and consist of huge data files. A major development in this regard has been the introduction of PACS (Picture Archiving and Communications System). It is a platform that allows for the integrated storage and viewing of medical images from diverse devices and systems. In the PACS server, images are mainly stored in the DICOM (Digital Imaging and Communications in Medicine) format.
DICOM is a standard developed by the American College of Radiologists. All images, including CT scans, MRI, ultrasound, and PET scans are to be stored, retrieved, and shared only in the DICOM format. The DICOM format has patient details embedded into the image to minimize diagnostic errors. A number of DICOM viewing applications are available on the market, and each has a different array of features that aid clinicians in diagnosis and treatment planning.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |
Another offshoot of 3D reconstruction is multiplanar reconstruction (MPR). MPR is the process of obtaining new slices of images from the 3D reconstructed model. The new slices are in planes different than for the slices that were originally acquired. This becomes particularly useful when tracking the course of major structures such as the aorta.
Imaging software today have multiple features to help healthcare professionals study their region of interest in detail. One such feature is intensity projection. Clinicians can choose to edit the image of a reconstructed area by displaying only the maximum or minimum CT values. These are called the maximum and minimum intensity projections, respectively (MIP and MINIP). They increase the contrast between the area of interest and the surrounding normal tissues.
3D reconstruction technology is still not as precise as we would like it to be, and some physicians prefer to go through multiple 2D sections to avoid errors. An interesting development in this area is ‘True’ 3D imaging. This innovative imaging system allows clinicians to view and interact with a virtual replica of an organ or body structure. The image appears in the form of a hologram, and clinicians can virtually rotate the structure, cut cross-sections, and identify vital anatomical landmarks. Such a tool could become indispensable for planning surgeries in the future.
An advanced medical imaging tool called image fusion is available in many DICOM applications. It allows the merging of two or more imaging datasets into a single file. This can combine the advantages of different imaging modalities. The most frequent and useful image fusion techniques are PET/CT and PET/MR image fusion, which combine the advantages of the PET scan, CT scan, and MRI. PET helps to identify and localize the area of interest (usually a malignant or inflamed area). CT provides excellent anatomical detail of the extent of the lesion as well as the tissue planes involved. MRI aids in achieving soft tissue resolution. When combined together, there is a remarkable increase in the sensitivity and specificity of diagnostic imaging investigations.
Traditionally, it has always been understood that there would be a ‘lag’ between the time the image is acquired and when it is interpreted. The lag comes from the time it takes to process and prepare the image, present it to the radiologist, and then for the radiologist to view each section of the image and apply their knowledge to interpret it. This lag can significantly impact clinical outcomes, especially in emergency situations such as trauma, where time is of the essence.
Today, many imaging systems offer ‘real time’ results, which means that the lag between image acquisition and interpretation is either minimal or none at all. Clinicians can view images on a screen while the patient is still in the imaging unit. This not only cuts down on lag, it has the additional benefit of viewing body systems at work in real time and thereby assessing their functional integrity. For instance, the swallowing function of the esophagus can be evaluated in this way for possible causes of dysphagia. Similarly, fetal movements can be seen in real time with ultrasound. The power of real-time imaging makes it possible for surgeons to make decisions intraoperatively.
Artificial intelligence (AI) refers to the ability of machines to simulate human intelligence. This mainly applies to cognitive functions, such as learning and problem solving. Within the context of medical imaging, AI can be trained to spot anomalies in human tissue—thereby aiding both in the diagnosis of diseases and monitoring their treatment. There are three ways in which AI can assist radiologists. AI can sift through huge datasets of images and patient information at superhuman speeds. This can expedite workflows. Secondly, AI can be trained to detect anomalies that are too small to be discerned with the naked eye. This can improve diagnostic accuracy. Thirdly, AI can be used to retrieve prior imaging scans from a patient’s electronic medical record (EMR), and then compare them with the patient’s latest scan results. Other aspects of the patient’s EMR, such as the any pertinent medical history, can also be retrieved and used to facilitate diagnosis.
Several companies have been successful in incorporating AI into imaging systems, but none of them are available for commercial use as of yet. One example of AI-integrated medical imaging software is Viz, which improves both detection and time to treatment in patients with large vessel obstructions (LVOs). The software is capable of screening multiple images across several hospital databases for LVOs. If an LVO is detected, the software can alert both the stroke specialist and the patient’s primary care physician to ensure that the patient receives prompt treatment. For a time-bound disease like stroke, this has the effect of greatly improving outcomes and reducing the cost burden on the healthcare system.
 - Created by PostDICOM.jpg)
Both the rapid advancement in imaging technology and the ubiquitous use of medical images in healthcare have resulted in an urgency to find innovative ways to store and share medical imaging data. Against this backdrop, cloud technology has emerged as one of the leading determinants of the future of medical imaging technology. Cloud technology enables the storage and sharing of data independent of geographic location with the help of the internet. Cloud-based medical imaging applications facilitate the storage and retrieval of imaging files in the DICOM format. They increase efficiency and decrease costs. Healthcare professionals can collaborate on medical imaging data from across the globe. The end result is better health outcomes for patients.
Cloud-based applications also improve the ‘blockchain’ process. A ‘blockchain’, in simple terms, is the addition of a new digital record to an old one, just like adding a new link to an existing physical chain. Images available on the cloud can be added to a blockchain, which then makes the patient’s medical information accessible to any physician anywhere around the world.
PostDICOM combines the best of the latest in medical imaging technology. It is one of just a few cloud-based DICOM viewing applications out there. The DICOM files stored on the cloud PACS server are secured with SSL encryption. PostDICOM incorporates medical 3D imaging technology and offers advanced image manipulation features, including multiplanar reconstruction, intensity projection (maximum, average, and minimum), and image fusion. Clinical documents can also be stored and viewed with the application. It is compatible with all major operating systems (Windows, Mac OS, Linus), and can be accessed from laptops, tablets, and smartphones. Best of all, for basic users, it is absolutely free to try cloud storage space.