
Just over a hundred years ago, the advent of X-rays was considered a significant leap in medical diagnosis. Over the last century, simple radiography has expanded into a specialized field—diagnostic medical imaging. X-rays have been harnessed using better technology via digitalized CT scans and new diagnostic medical imaging techniques, such as the MRI and ultrasound, have emerged. Medical imaging modalities continue to evolve and refine. As the actual imaging process progresses, there is a parallel, and equally important, improvement in the handling of medical images and the associated workflow. In this article, we zoom in on the most important advances in medical diagnostic imaging that have transformed the way physicians examine and treat patients.
Medical imaging is used primarily to diagnose diseases as well as to monitor their progress. It is essential that the images produced are of the highest quality since they have a direct bearing on patient outcomes. To maintain quality, a set of standards for medical images was developed jointly by the American Society of Radiology and the National Electrical Manufacturers Association. It is referred to as the DICOM standards, which stands for Digital Imaging and Communications in Medicine. Images produced by all medical imaging hardware must conform to the characteristics described in this standard. Furthermore, there is a specific format available for storing and sharing medical images—referred to as the DICOM format.
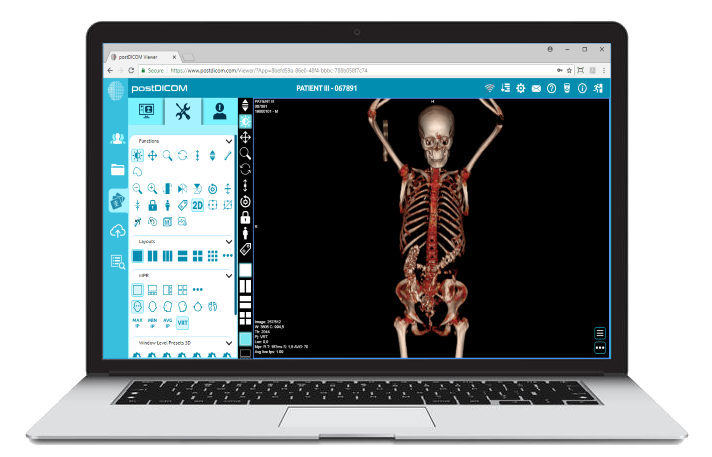
All medical imaging equipment manufactured today is supposed to conform to the DICOM standards. Viewing of the images thus produced cannot be done by ordinary imaging programs available on a regular PC. A special diagnostic medical imaging program is required, known as a DICOM workstation. For commercial use in medical diagnosis, such diagnostic medical imaging programs need to be FDA approved and need a special license. These measures ensure that any application developed for clinical purposes is capable of accurate depiction of high quality medical images.
With the arrival of digitalized medical diagnostic imaging, the need to develop X-ray films has markedly declined. However, digital images are still being converted into ‘films’ with the aid of printers. Imaging films require proper storage under the right conditions to prevent damage over time. Retrieval of these images from storage can be a time consuming process and requires dedicated personnel for record-keeping.
PACS, which stands for Picture Archiving and Communications System, obviates the need for physical storage and retrieval of films. It is basically a platform for the virtual storage and retrieval of medical images. PACS makes it possible to handle enormous volumes of data related to medical images. Any computer that is connected to a specific PACS server is able to retrieve DICOM images and view and even modify them. The latest innovation has been the introduction of cloud-based PACS, where instead of local storage, the PACS is hosted on the internet and any user connected to the internet, with the right credentials, can access the images.
Not only has PACS simplified storage and retrieval, it has also made teleradiology a reality. Today, radiologists need not be present in the same area where images are being acquired. They can view images from different geographic locations and provide their expert opinion. Through teleradiology, a single radiologist can generate reports for images coming in from multiple hospitals. This saves precious time and resources, and helps to reduce healthcare costs.
With the need for developing or printing of films gone, the workflow process for acquiring and viewing medical images has improved. Real-time imaging is a concept where there is no time lag between the acquisition of images from the patient and their viewing by the physician. Radiologists can literally view images while the patient is still within the scanner.
The faster interpretation of diagnostic medical images leads to immediate diagnosis, which in turn enables rapid medical intervention. Real-time medical diagnostic imaging plays a significant role in emergencies. For instance, in trauma patients, intra-abdominal injury was earlier determined by diagnostic laparoscopy or peritoneal lavage, both of which were invasive procedures. Today, however, the standard of care is to use FAST (Focused Abdominal Sonography in Trauma), which uses a real-time ultrasound to quickly determine whether or not a patient has suffered an intra-abdominal injury. Real-time ultrasound imaging is also used to monitor the health of the fetus in utero and assess growth parameters.
Most diagnostic medical imaging systems are designed to diagnose anatomical or structural abnormalities. Modern medical diagnostic imaging, in addition to that, can also assess abnormalities in tissue and organ function. This includes detection of abnormalities in physiological processes such as metabolism and blood flow. Functional imaging is largely achieved through nuclear medicine. Nuclear medicine is a speciality of radiology which involves injection of molecules that are ‘tagged’ radioactively into the body. These radioactive molecules may be preferentially taken up by specific organs for various physiological processes. After uptake, the organs can emit radiation, which is picked up by external scanners as ‘hot spots’. For instance, positron emission tomography (PET) reflects the uptake of radiolabeled glucose by cells. Cells that have increased metabolic activity, in particular cancer cells, tend to take up more glucose. This technique is therefore used to identify areas of metastasis within the body. Another functional imaging technique is the use of thyroid scans, which are used to detect hyperthyroidism. These scans depend on the uptake of radioactive iodine by thyroid cells.
Most functional imaging techniques, when used alone, can be difficult to interpret. This is because although they detect areas of abnormal physiological activity, it can be difficult to orient these areas anatomically. This may be overcome by a technique called image fusion. Modern diagnostic medical imaging programs allow fusion of two or more diagnostic techniques. For instance, fusion of a PET scan with a CT scan can help identify whether or not there is metastasis, and can also precisely identify the anatomical zones in which metastasis has occurred.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |
Post-processing techniques refer to interventions applied to diagnostic medical images after the images have been acquired from the patient. Post-processing techniques are usually done using an advanced diagnostic medical imaging program. They provide the radiologist with information that is not available by just looking at the original images. Some of the most useful post-processing techniques used in medical diagnostic imaging are as follows:
3D reconstruction: A critical drawback of medical diagnostic imaging is that it is two-dimensional in nature. Nevertheless, recent technology allows images to be viewed as three dimensional objects, by taking multiple image slices and stacking them together. This allows better anatomical orientation and is easier to interpret. It also helps to understand the relationship between various structures. Another form of 3D reconstruction is multiplanar reconstruction. In this, the radiologist can take the 3D object, rotate it at will, and slice at any given angle, different from the originally acquired slices. These techniques help the radiologist virtually view the anatomical structure as if they were physically holding and slicing it, giving them an unmatched level of accuracy.
Intensity projections: This is based on the premise that different structures within the body will absorb and reflect different amounts of radiation, which would be reflected in their CT numbers. In maximum intensity projections (MIP), only regions that have the highest CT numbers are displayed. MIP is most useful in CT angiography, where it helps to distinguish large blood vessels from other anatomical structures. In minimum intensity projections (MINIP), only the regions that have the lowest CT numbers are displayed. MINIP is extremely useful in lung parenchyma diseases, which present as hypo-attenuated CT values. For instance, in patients with constrictive obstructive bronchiolitis, CT changes are extremely subtle. Using MINIP can make these changes more conspicuous.
Artificial intelligence (AI) is an exciting front that is slowly making inroads into medical diagnostic imaging. Artificial intelligence is the ability of machines to make cognitive decisions, such as learning and problem solving. By feeding computers deep learning algorithms, they can learn to distinguish between various digital patterns and can thus aid in diagnosis. A team of researchers at Stanford University, for instance, has developed such an algorithm for chest X-rays. The researchers claim that by using this algorithm, computers can recognize the presence or absence of pneumonia better than radiologists. The radiology team at UCSF meanwhile is partnering with GE to develop a series of algorithms that can help distinguish between normal and abnormal chest X-rays. Another medical application, called Viz, helps screen multiple images across several hospital databases for large vessel obstructions (LVO), which are indicative of imminent stroke. If an LVO is detected, the software can alert both the stroke specialist and the patient’s primary care physician to ensure that the patient receives prompt treatment.
While PACS stores medical images, other medical information is stored in different systems. For instance, health information systems (HIS) store information related to the patient’s medical history, clinical details, and laboratory investigations. Radiology information systems (RIS) manage imaging data apart from the actual images, such as referrals, requisitions, billing details and interpretations. All these information systems are separate from each other. Yet, in dealing with a patient, a physician must often have all these details together on hand to make a diagnosis and plan treatment. Integrating all information systems into a single medical record that can be accessed through a single server can help streamline workflow and improve both accuracy and throughput.
Rising healthcare costs: As diagnostic medical imaging continues to stride ahead, each new development comes at a cost. The cost of the technology itself, the cost of research and the cost of implementation are finally reflected as one parameter—the increased cost of healthcare to the patient. Perhaps, this is why developing nations still rely on manual X-ray imaging and manually developed films for diagnosis of basic diseases, and reserve advanced imaging techniques for more complex health conditions. Still, if everyone is to benefit from advances in diagnostic medical imaging, efforts must be made to keep the cost of new medical technologies at affordable levels.
Protection of patient data and privacy: As diagnostic medical imaging relies more heavily on web-based technologies, patient information gets uploaded and stored online. There is some basic protection in place, in that only specific user accounts which are owned by physicians and hospitals can access PACS servers. When images are exported for purposes of teaching or research, there is an option to anonymize data that could be used to identify patients. Even so, there have been concerns about data breach and loss of patient privacy. There is an urgent requirement for policy measures to be taken that will ensure protection of medical imaging data on PACS servers.
PostDICOM helps you and your practice keep pace with the ever-evolving landscape of advanced diagnostic imaging. This robust, yet easy-to-use diagnostic medical imaging program is a modern DICOM image viewer with several advanced features. PostDICOM offers a cloud-based PACS platform and is supported on multiple operating systems including Windows, Mac OS, Linux and Android. It allows you to access your DICOM files anywhere, from any device. PostDICOM has sophisticated post-processing tools that enable superior diagnosis and treatment planning. While our PACS is cloud-based, patient data is completely secure. We keep patient data separated by geographical regions, all data is encrypted, and secure SSL systems are used for communication. Images can be anonymized before uploading to the PACS server. PostDICOM is free to try with all features for limited time! Storage can be upgraded at a nominal cost. To harness the power of advanced medical imaging, visit postdicom.com and try your free viewer today!