 - Created by PostDICOM.jpg)
Medical imaging today has advanced to the point where it is impossible to think of running a healthcare facility without the utilization of several different imaging modalities. In order to maximize the benefits offered by medical imaging, it is imperative to understand the fundamentals of various types of medical imaging scans. In this article, we will discuss the two major types of medical scan and imaging technology behind them.
CT stands for computerized tomography. In medical imaging, CT scan is one of the most commonly performed scans for diagnostic purposes. In simple terms, the CT scan uses a rotating X-ray machine, which is capable of taking images of your body from several different angles. Like X-rays, it uses radiation energy, which is absorbed and reflected to different degrees by different structures of the body.
The CT machine consists of a circular, donut shaped device, called a gantry. The patient lies down on an imaging table, which then slowly passes through this gantry. There is a motorized X-ray source that rotates all around the circumference of the gantry, emitting several narrow X-ray beams. As a specific body part crosses the tunnel, X-rays enter the body in all directions. Once the X-rays pass through the body, they are picked up by special digital X-ray detectors, rather than films. The X-ray detector within the CT scanner is more sensitive than the traditional X-ray film, and can pick up several degrees of distribution density.
The data from the detector is then transmitted to the computer. Data obtained from one complete rotation of the X-ray source is reconstructed using mathematical techniques. The reconstructed image appears as a two-dimensional, cross sectional image ‘slice’ of the body part. Each slice can vary from 1 mm to 10 mm in thickness, depending on the type of machine used. The next rotation of the source brings out a different slice of the body. Several such rotations occur, until a series of slices representing the entire body part is obtained. These slices may be stacked together to obtain a three dimensional image of the body part.
 - Created by PostDICOM.jpg)
Reading CT scan images requires a good knowledge of anatomy and a sound sense of the orientation of different body structures. It requires a few years of training and study to learn how to properly interpret a CT scan and make a clinical diagnosis from it. However, it is always helpful to keep the following tips in mind when a CT scan is being interpreted:
Most CT images are presented in the transverse or axial section. Imagine the patient’s body as being divided into several slices, using a cutting disc that is parallel to the ground surface. You would be looking at one of these slices as though you are lying on the floor, staring upwards.
To get your bearings, hold the film in front of you and begin at the part of the image that lies in the 9 o’clock position. This is right, 12 o’clock is anterior, 3 o’clock is left, and 6 o’clock is the posterior part of the cross-section.
Once you are oriented to the plane and direction, begin identifying different structures present in a single cross-section. Knowing the ‘color’ that a particular structure takes on is helpful during identification. Various tissues in the body absorb different amounts of radiation, and emit the rest. The amount of absorbed radiation is measured as Hounsfield Units (HU). Tissues with a greater number of Hounsfield Units appear whiter than the rest, while tissues with a lower HU value appear blacker. For instance, air does not absorb any radiation (-1000 HU), and so appears completely black. Bone, on the other hand, absorbs radiation completely (1000 HU) and appears completely white. Water (0 HU) appears grey. Fat is a darker shade of grey than water (-70 HU), while blood is a lighter shade of grey as compared to water (70 HU).
MRI stands for magnetic resonance imaging. It is a form of medical imaging that does not require the use of radiation. Instead, it uses a combination of powerful magnetic fields, radio waves, and computerized technology to create a detailed image of your body structures.
MRI works on the principle that your body is largely made up of water. Water consists of hydrogen and oxygen atoms. The hydrogen atom, which is made up of a single proton and an electron, reacts to the process applied during an MRI scan.
The MRI machine consists of a tunnel-like closed tube, in which the patient lies during the procedure. This tube houses a powerful electromagnet. When the patient lies within the electromagnetic field, the hydrogen atoms inside the patient’s body have a tendency to align themselves parallel to this magnetic field. Next, high frequency radio waves are applied across the magnetic field. When these radio waves strike the hydrogen atoms, the protons get excited, and they begin to spin, losing their alignment. When the radio waves are turned off, the protons attempt to re-align themselves to the magnetic field. In doing so, the protons give off the excess energy they gained in the form of an electric signal. This is picked up by the MRI sensor and processed to form a digital image on the computer.
 - Created by PostDICOM.jpg)
When you read about MRI machine images, you may have heard of the terms T1-weighted sequences and T2-weighted sequences. This terminology comes from the type of MRI pulse sequences applied to the radiofrequency waves that are used to create the MRI images. These sequences actually determine what does an MRI image look like. In a pulse sequence, different parameters can vary. Some of these parameters include:
Time to repetition or TR: This is the time taken from the application of one excitation pulse to the next excitation pulse. If the TR is long, the protons have enough time to relax and re-align themselves to the magnetic field. If the TR is short, the protons do not relax back fully, and the electric signal they release will be decreased.
Time to echo or TE: This is the time at which the electrical signal that is released from the spinning protons is measured. The longer the TE, the more likely it is that the electric signal will be reduced, as the protons would have gone back to their alignment.
T1-weighted sequences are most commonly employed in MRI protocols. These sequences have short TEs and short TRs. T1-weighted sequences create images that are easy to interpret anatomically. In T1-weighted sequences, various tissues take on different appearances, as follows:
Fat has high signal intensity and appears white.
Fluids (such as cerebrospinal fluid and urine) have low signal intensity and appear black.
Muscle has intermediate signal intensity and appears grey.
Brain: The grey matter has intermediate signal intensity and appears grey. White matter has slightly more signal intensity and appears whitish-grey.
Paramagnetic contrast agents, like gadolinium, appear white. When using the gadolinium contrast in an MRI, it is possible to use a ‘fat suppressed’ T1 sequence, so that the contrast material may be easily distinguished from fat, as both of these appear white.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |
T2-weighted sequences have long TRs and long TEs. In T2-weighted sequences, tissues have the following appearances:
Fluids (such as cerebrospinal fluid and urine) have high signal intensity and appear white.
Muscle has intermediate signal intensity and appears grey.
Fat has high signal intensity and also appears white but is less white as compared to its appearance in T1 images.
Brain: The grey matter has intermediate signal intensity and appears grey. White matter has slightly lesser signal intensity and appears darker grey in color.
T2-weighted sequences can also be taken in the fat suppressed mode. This allows the detection of edema or inflammatory fluid in fatty tissues. In addition to this, there is another mode called the ‘fluid attenuation’ mode. In this mode, the signal coming from normal body fluids is suppressed. This is useful in the detection of brain edema, where the signal coming in from cerebrospinal fluid would be suppressed.
A special form of T2 sequencing is used in magnetic resonance cholangiopancreatography (MRCP), in which the TE is extremely long. This allows the signal to be lost from most tissues, and only tissues which retain the signal for long periods of time, such as fluid-filled structures, would be detected. This usually occurs with structures in the abdomen, which appear more hyperintense than the surrounding structures, and this allows them to be easily distinguished.
CT and MRI imaging are the most frequently used imaging modalities, and patients as well as healthcare workers may sometimes find it difficult to choose between the two. However, they are distinct imaging options. Some salient features tell us how to tell the difference between MRI and CT images:
| Feature | CT Scan | MRI Scan |
| Health risks | CT scans use ionizing radiation. This is not suitable for use in high risk groups, like pregnant women | No radiation is used. However, it is dangerous to use in people with pacemakers, artificial joints, or other metallic implants that can be affected by the electromagnetic field. |
| Tissue detail | Excellent bony anatomy Poor soft tissue detail |
Excellent soft tissue detail Poor bony anatomy |
| Time taken | Usually 5 to 7 minutes; suitable for emergency imaging | Takes 30 to 45 minutes; not suitable in emergencies |
| Patient comfort during the imaging process | The process is reasonably comfortable | The imaging process is extremely noisy and takes place in a closed chamber, which may not be acceptable for claustrophobic patients |
| Cost | Approximately $1200 | Approximately $2000 |
The above mentioned distinguishing features should help the physician choose the more appropriate imaging modality in a particular clinical situation.
 - Created by PostDICOM.jpg)
CT imaging is useful for spot diagnosis and in emergencies. Some of the common applications of CT imaging are highlighted below:
Bone fractures and other problems: CT scans can be used to detect fracture lines in bone, and to detect erosion of bone by anatomical or pathological structures.
Pathological lesions: CT is useful to detect pathological anomalies, such as cysts and tumors. It can detect the extent of invasion of malignant tumors.
Bleeds and vascular lesions: CT can detect internal bleeds, such as intracranial or subarachnoid haemorrhage. It can also be used to identify aneurysms and atherosclerotic lesions. This is useful in emergencies, such as stroke, where immediate management is required.
In medical imaging, MRI is more useful when clearer images are needed and greater detail must be visualized. Some of the common applications of MRI imaging are highlighted below:
Joint imaging: MRI can be used to view articular disc displacements. They can also detect ligament or tendon tears and detachments.
Brain and spinal cord imaging: MRI can detect herniation of spinal discs, multiple sclerosis, and other brain conditions.
Bowel and abdominal imaging: MRI can be used to image conditions, like inflammatory bowel disease, and liver cirrhosis.
 - Created by PostDICOM.jpg)
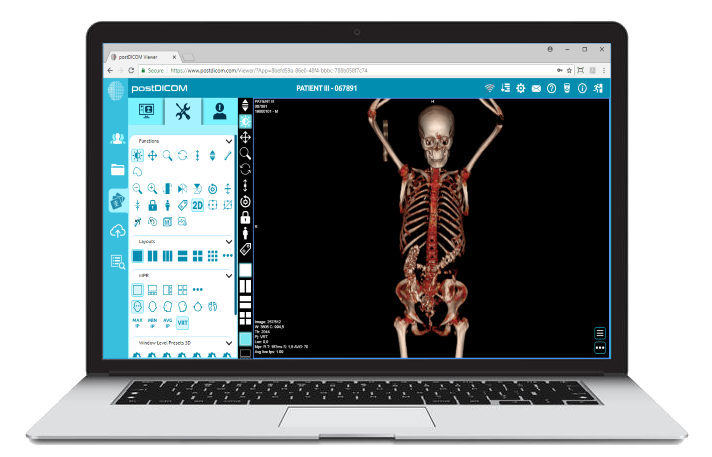
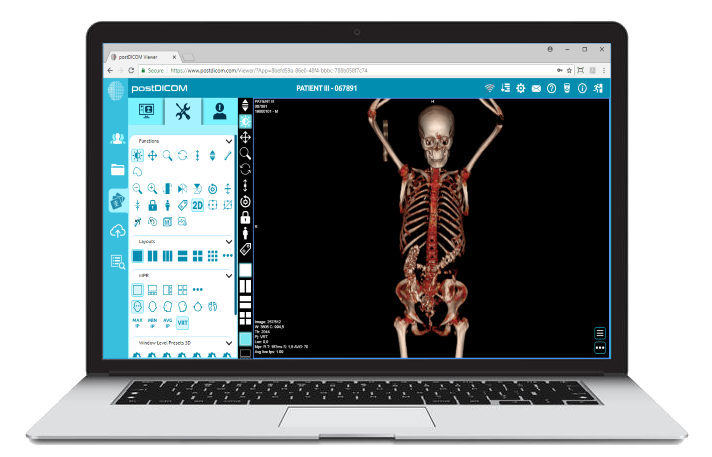
CT and MRI images are acquired in a special digital format, called the DICOM format. DICOM ensures that the high quality of the images is retained. Each CT or MRI scan contains multiple images in the DICOM format that need to be stored in a safe and secure manner.
To store such a large volume of medical images, each hospital usually has a PACS server. PACS (Picture Archiving and Communication System) is a central server on which images are stored, and from which they can be retrieved when needed. Usually, hospitals have an on-site, standalone PACS, and invest plenty of money into upgrading the storage capacity of the PACS when it gets full. Back-ups can come at a higher cost.
PostDICOM’s cloud-based PACS solutions offer convenient, off-site storage for DICOM images. Because DICOM files are hosted on the internet, they are safe from data loss and can be accessed from any device. Cloud-based PACS have three layers of security, so patient data remains confidential.
PostDICOM’s cloud-based PACS is much more economical than standalone PACS solutions! When you sign up, you can have a trial period and use cloud storage completely free. Additional storage can be purchased for nominal costs, and you can upgrade or downgrade your subscription at any time, based on your storage needs. PostDICOM also lets you view stored DICOM files for free, with our online, zero-footprint DICOM image viewer. So, get the most out of CT and MRI imaging by signing up for PostDICOM’s cloud storage solution today!
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |