Gone are the days when grainy X-ray film used to be considered cutting-edge medical imaging.
From detailed CT scans to real-time ultrasound technology, diagnostics now reveal internal anatomical intricacies previously impossible.
Yet for all the visual clarity modern modalities provide, peering into anatomical abnormalities and comprehending complex biochemical processes underpinning diseases like cancer long relied on cruder nuclear imaging approaches.
But with recent advances in radiotracer analytics plus digitized image management systems, nuclear technology is now experiencing its own revolution.
We will go through the synergistic rise of Positron Emission Tomography (PET) for precision tracer imaging alongside Picture Archiving And Communication Systems (PACS) centralizing scan storage/analysis.
Nuclear medicine has entered a new era where life-saving visualizations accelerate everything from clinical trial inclusion to tumor radiation therapy planning.
Stay with us to learn the details!
Long before MRI and CT scans produced detailed anatomical renderings, nuclear medicine emerged using radioactive tracers targeting bodily processes otherwise invisible.
Yet early gamma cameras lacked specificity, differentiating tumor spread from healthy inflammation. Enter positron emission tomography (PET), a game-changing technology significantly advancing nuclear imaging’s capabilities.
But what exactly is PET, and why should healthcare leaders care?
PET imaging involves injecting patients with biologically active molecules containing radioactive tracers like fluorodeoxyglucose (FDG) that accumulate in areas of heightened metabolic activity.
The PET scanner’s gamma-ray detectors then create 3D images pinpointing tracer concentrations. This identifies abnormalities at the molecular level earlier than density discrepancies detectable by CT/MRI alone.
Whole-Body Perspective: Unlike CT/MRI, which are confined to imaging single areas, PET scans capture systemic views that help evaluate cancers that commonly spread. Finding isolated active lung lesions otherwise missed has huge treatment implications.
Enhanced Specificity: Certain radiotracers attach specifically to malignant tumor processes, better-differentiating malignancy versus inflammation, often indistinguishable on CT or MRI. This specificity allows more targeted care.
Rapid Results: PET scans require under an hour rather than most CT/MRI exams spanning 30 minutes to over an hour for equivalent coverage with longer physician review time. This supports prompt clinical decisions.
Assessing Effectiveness: Following cancer treatment cycles by repeating PET offers quantitative guidance on therapeutic response. For example, seeing metabolic activity changes post-radiation helps clinicians calibrate ideal interventions per patient.
Oncology: Characterizing suspicious masses, staging cancers, and monitoring therapies or remission status all employ PET imaging today as the standard of care for many malignancies like lymphoma. This expansion relied upon the versatility molecular targeted tracing provides.
Neurology: PET helps evaluate seizures, memory disorders like Alzheimer’s disease, and even psychiatric conditions by revealing metabolic patterns, offering diagnostic clues unavailable through conventional imaging tests.
Cardiology: PET can map heart tissue viability after heart attacks, showing zones that may still be salvaged by prompt intervention more clearly than MRI alone. This application is still under development but shows immense promise.
As diagnostic imaging volume explodes with ongoing modalities adding PET alongside traditional X-ray, CT, and MRI scans, efficiently managing exponential exam quantities grows increasingly untenable using outdated film archives.
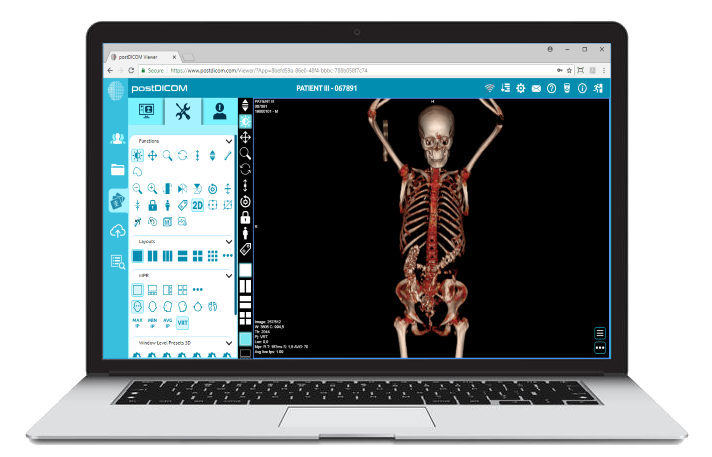
Enter the picture archiving and communications system (PACS) - a revolutionary digital image capture/analysis framework fast becoming indispensable infrastructure across radiology and beyond.
Simply put, PACS replaces film to digitize imaging workflow. Exams are directly transferred from scanners into centralized storage databases with backup tools protecting perpetual access.
Integral DICOM viewers enable multi-stakeholder image analysis, annotation, and reporting. Compared to films risking fading, physical degradation, or accessibility limits, PACS systems facilitate streamlined productivity.
Instant Accessibility: Authorized radiologists, technologists, referrers, and surgeons can access studies immediately from anywhere, eliminating physical transport delays. Cloud hosting further bolsters ubiquitous mobile availability.
Collaborative Interpretation: Integrated tools allow multi-specialist image consults in real-time regardless of viewer proximity, enabled by digital transfer conveniences.
Structured Data and Metrics: DICOM data standardization allows monitoring key benchmark indicators like report turnaround times, supporting improved outcomes.
Patient History in Context: Consolidated archives containing all exams provide crucial clinical context aiding diagnostic accuracy, unlike episodic film conditions. Longitudinal case reviews further clinical education.
Research Applications: Deidentified images fuel big data research, elucidating trends across population health analytics, clinical trials, and beyond to accelerate medical discoveries through expanded datasets.
Enterprise Integration: Interfaces linking PACS directly with electronic medical records (EMRs), laboratory, pharmacy, and billing systems maximize efficiency with automated documentation pushing rather than the manual pull needed for siloed film records.
This centralized, integrated command center concept through PACS propels imaging beyond isolated snapshots toward interconnected efficiency gains.
As analytics and automation synergies continue maturing, the technology trajectory converges upon elevated imaging insights rather than any feared functional declines.
From private practices to leading university hospitals, healthcare organizations integrating positron emission tomography (PET) and picture archiving communications systems (PACS) gain measurable operational and clinical advantages, including:
Consolidating enterprise imaging assets into efficient PACS structures streamlines exam workflow by abolishing film transport while pushing instant availability.
Combining multi-department data from PET, CT, X-ray, MRI, and beyond under a universal interface prevents redundancies like re-entering demographic data repeatedly.
With robust datasets aggregated spanning years of images matched to metadata like diagnoses and case progression, powerful data mining potential unlocks for administrators.
Hospitals can analyze performance patterns by adjusting staffing needs or better negotiate insurance payer contracts backed by quantifiable imaging utilization metrics.
Having integrated PET findings available within universal viewers creates an opportunity for earlier intervention planning based on subtle molecular changes identifiable before anatomical aberrations appear.
This allows coordinating surgery, radiation therapy, or palliative care ahead of later-stage pressures.
Standardized DICOM quantitative data extracted from PACS and curated deidentified images accelerates everything from publishing studies to attracting pharmaceutical trial sponsors.
Quickly screening study cohorts using historical scans facilitates optimal trial enrollment aligned to biomarker prerequisites.
Shared viewer spaces allow radiologists, oncologists, cardiologists, and other specialists to consult imaging studies with real-time notation simultaneously. This interdisciplinary perspective exchange matters greatly for complex pathology interpretations.
Even outside acute contexts, value emerges from informal case review discussions across specialty lines.
In essence, PET/PACS integration converges multiple benefits - clinical, operational, and financial - to elevate medical imaging beyond isolated images toward more collectively actionable visual intelligence benefitting individual patients and overall population health outcomes.
While productivity and diagnostic enhancements rightfully grab provider mindshare adopting integrated medical imaging ecosystems, the ultimate beneficiary remains the patient.
By exploring the key benefits cross-linked PACS and PET care delivery models unlock, individual well-being implications reveal why this digital shift matters.
Consolidating years of patient imaging history plus specialized PET scans under universally accessible archives arms radiologists with information-rich clinical context.
Rather than solely relying on isolated CT findings, multi-modality perspectives confirm pathology much faster, and catching cancers sooner before they spread saves lives.
Since all images are stored perpetually in connected frameworks, repeat scans for lost films or seeking past comparisons decline significantly. This reduces radiation exposure and expensive duplicate procedures when timeliness trumps prudence.
Emerging algorithms will soon automatically flag history, possibly answering clinical questions without added scanning.
Between simplified scheduling tapped straight into EMR records plus digitized intake workflows and mobile-friendly exam prep materials, onboarding patients grows more seamlessly amidst connected infrastructure.
Following tests, automated report distribution into patient portals prevents anxiety around results delivery waits. Convenience and education matter for positive perceptions.
As threats like ransomware attacks threaten vulnerable medical centers, leading PACS solutions incorporate cloud-based backup with end-to-end data encryption, safeguarding mission-critical imaging assets and patient privacy should disaster strike.
Some firms guarantee 100% uptime or compensate customers for breach harm, contractually assuring confidence.
Of course, the greatest assurance comes through health restored. However, patient experience peripherals enabling that outcome contribute significantly. “I never felt lost in the shuffle even as hospital shifts changed,” one satisfied cardiac surgery patient notes. “The doctors somehow still knew my case inside and out, thanks to the pictures they'd discussed as a team. I'm grateful for that.”
While interconnectivity promises abound merging multimodality medical imaging under shared platforms, seamless integration rarely unfolds without overcoming expected complexities, including:
Linking disparate technologies tries the patience of even seasoned IT experts. However, reputable PACS vendors provide tested application programming interfaces (APIs) readily connecting major scanner models and smoothing data flow fires before flaring.
Cloud-native PACS also circumvent server compatibility issues.
As workflows shift from analog film transportation towards analyzing digital dashboards, team skills also demand adjustment through retraining.
Radiology technologists grow into broader data curation roles while physicians and surgeons master remote collaborative tools. Proactive change management prevents setbacks.
Financial forecasting integrations combine device expenses, software subscriptions, training costs, and more convolute budget planning.
But trusted vendors provide transparent pricing models backed by reputable hospital case studies confirming ROIs averaging under 3 years across $2-10 million installations even before accounting for patient experience and workplace culture boons.
Replacing vast film libraries with streamlined servers frees up infrastructure for revenue-generating clinical expansion.
Forward-looking healthcare leaders view this flexibility as a strategic asset for attracting revenue-driving modalities like PET rather than mourning abandoned shelves. Form follows function.
While connecting disparate data flows introduces ethical questions, leading PACS ADMINS monitor user access stringently through role-based authorizations, access logs, and consent directives to uphold patient rights during exponential growth.
Privacy preserves trust even amidst digital transformation.
By acknowledging foreseeable integration speedbumps stemming from system scale rather than isolated applications alone, imaging modernization navigator's chart courses circumvent hazards in favor of secure progress.
No singular solution addresses all imaging inefficiencies, but consolidating through PACS and PET partners propels your patients in a positive direction.
 - Created by PostDICOM.jpg)
If hybrid imaging proves it possible to link anatomical form with biochemical function, projecting integrated diagnostic futures reveals bolder realities nearing through continued technological momentum.
From augmented analytics to enhanced isotopes, let’s explore pending innovations that stand to redefine PACS and PET capabilities further:
Expect algorithms to automate tedious tasks like image segmentation for the region of interest enhancement or data reconstitution, improving quality.
Machines can also scrub studies for protocol adherence, and eventually, self-learning quality control correlates with optimizing human reviewer capacity five-fold.
Pharmaceutical researchers expand tracer libraries to target intricate processes like PSMA monitoring prostate cancer genes.
Concurrently, newer PET CTs feature expanded detector sensitivity and 3D reconstruction, improving anomaly detection. Combining targeted isotopes with ultra-definition readings heightens insights.
Rather than subjective qualitative reads alone, standardized uptake values (SUVs) provide objective metrics for tracing disease progression change over time and assessing treatment efficacy by changes in metabolic activity. This unlocks evidence that can guide clinical trial recruitment.
Capturing scan volumes, radiopharmaceutical usage, and radiologist sub-specialization metrics builds dashboards connecting images to business intelligence for maximizing resource planning, including staffing, machine investments, and patient experience enhancements.
Augmented overlays superimposing patient monitors onto scanning windows during PET procedures bolsters tech ergonomics and information handoffs. Portable PET solutions break mobility barriers beyond fixed trucks, enabling bedside and remote diagnostics.
Together, this amalgamation of enhanced connectivity, processing prowess, and clinical customization spotlights a future where nuclear detections enable practitioners to peer clearly into patient molecular pathways far beyond superficial scans alone.
An open, integrative infrastructure propels access beyond physical facilities into decentralized precision guidance, improving individual outcomes through properly processed particulate proxies.
As healthcare continues prioritizing preventative precision and predictive accuracy, molecular imaging adopting integrated platforms like PACS-synced PET scanners shifts diagnosis towards curative collaboration between anatomical shape and biochemical contributors underneath disease.
Quantifying patterns across structural and functional visuals furnishes practitioners with expanded insight while consolidating access and analytics unlocks enterprise efficiencies from tech managers to hospital administrators.
Most importantly, patients receive expedited answers and enhanced care as enterprise imaging ecosystems bridge specialists under shared visual language and instant availability.
While legacy nuclear modalities rely on crude static scans, the new era convergence with clarified visualization and connected workflows propels medicine into previously impossible individual and population health gains.
By merging molecular sight with digitized specialist collaboration, PACS-PET integration ultimately revolutionizes nuclear medicine’s future today.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |