
In a dimly lit room, radiologist Dr. Martinez recalls the early days of her career, squinting at grainy X-ray films, trying to discern subtle abnormalities.
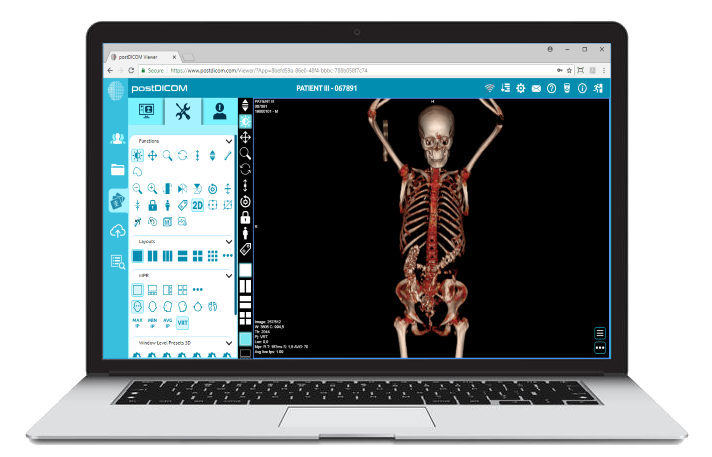
Fast forward to today, and she's navigating through a 3D rendering of a patient's spine, rotating it, zooming in, and viewing it from multiple angles, all with a few clicks.
The world of medical imaging has undergone a seismic shift, with advanced image processing tools at the forefront of this revolution. Recent studies suggest these tools can enhance diagnostic accuracy by up to 30%.
As we stand on the cusp of a new era in diagnostics, let's delve into how these cutting-edge tools are not just refining images but reshaping the fabric of healthcare.
The inception of medical imaging can be traced back to the late 19th century with the discovery of X-rays. These rays, capable of penetrating human tissue, unveiled a world previously hidden from the naked eye.
Radiographs, or X-ray images, became the first step in visualizing the body's internal structures. However, these early images were often grainy and lacked detail. While revolutionary, they presented clarity, precision, and depth challenges.
Diagnosing conditions required a keen eye and often left room for interpretation, leading to potential inaccuracies.
As medical science progressed, the need for clearer, more detailed images became evident. Traditional imaging techniques, though groundbreaking, had their limitations. They often provided two-dimensional views, lacked contrast in certain areas, and could not capture dynamic processes within the body.
For instance, visualizing blood flow or understanding the intricate structures of the heart was beyond the scope of essential imaging. These limitations often meant that conditions went undetected or were misdiagnosed, emphasizing the need for more advanced imaging solutions.
Enter the era of advanced image processing. With the convergence of technology and medicine, tools were developed to enhance, refine, and manipulate medical images. These tools went beyond just capturing images; they allowed for multi-dimensional views, detailed layer-by-layer analysis, and even real-time visualization of bodily processes.
Technologies like computed tomography (CT) and magnetic resonance imaging (MRI) emerged, offering slices of images that could be reconstructed in various planes. Software advancements further propelled this evolution, introducing algorithms and tools to highlight specific areas, enhance contrasts, and provide unparalleled clarity.
The transition from primary to advanced imaging marked a new dawn in diagnostics. The limitations of traditional imaging no longer restrict healthcare professionals.
They now had a suite of tools, enabling them to dive deeper into the human body, uncovering previously elusive insights. This shift enhanced diagnostic accuracy and paved the way for personalized treatment plans tailored to each patient's unique needs.
In medical imaging, viewing structures in various planes is invaluable. Multi-Planar Reconstruction, or MPR, offers precisely this capability. Unlike traditional imaging that provides a singular, often flat perspective, MPR allows healthcare professionals to reconstruct images in multiple planes, be it axial, sagittal, or coronal.
This means that a radiologist can view an organ or tissue layer by layer, gaining a comprehensive understanding of its structure and any potential anomalies. MPR's significance lies in its ability to offer a three-dimensional perspective from two-dimensional image slices, enhancing diagnostic accuracy and providing a more holistic view of the area of interest.
Detecting abnormalities often requires a keen eye, especially when they are subtle. Maximum Intensity Projection, commonly known as MIP, is a tool designed to aid this process. MIP projects the brightest pixel value in a particular view onto a 2D image.
In simpler terms, it highlights the most intense areas, making structures like blood vessels or bone abnormalities stand out. For conditions where contrast is crucial, such as in angiography, MIP is an indispensable tool, ensuring that even the minutest details are not overlooked.
While MIP focuses on the brightest areas, MINIP (Minimum Intensity Projection) and AVGIP (Average Intensity Projection) offer different perspectives. MINIP emphasizes the darkest pixels, making it particularly useful in visualizing air-filled structures like the lungs.
On the other hand, AVGIP calculates the average intensity of pixels, providing a balanced view that's especially beneficial in areas with varying densities. Together, these tools offer a spectrum of perspectives, ensuring that healthcare professionals comprehensively understand the imaging area, irrespective of its density or composition.
One of the most visually striking advancements in medical imaging is 3D rendering. Moving beyond flat, two-dimensional images, 3D rendering allows for the visualization of structures in three dimensions. This provides a more realistic view and enables the image's rotation, zooming, and manipulation.
Whether it's understanding the intricate pathways of the heart or visualizing the architecture of a bone, 3D rendering offers unparalleled clarity and depth. Its significance extends beyond just diagnostics; it's also a valuable tool in patient education, allowing individuals to visualize and understand their conditions better.
In a renowned cardiology center, Dr. Patel faced a challenging case. A patient presented with unexplained chest pains, and traditional imaging methods yielded inconclusive results. Turning to Maximum Intensity Projection (MIP), Dr. Patel highlighted the blood vessels in the heart, revealing a subtle vascular anomaly that was previously overlooked.
This discovery pinpointed the cause of the patient's discomfort and allowed for timely intervention, preventing potential complications. This case underscores the transformative potential of MIP in detecting vascular issues, ensuring that even the most subtle abnormalities are brought to light.
A patient with persistent respiratory issues posed a diagnostic challenge at a pulmonary clinic. While X-rays and essential imaging provided some insights, the root cause remained elusive. Employing MINIP, the pulmonologist emphasized the air-filled structures of the lungs.
The resulting images unveiled tiny airway obstructions that were the culprits behind the patient's symptoms. With this clarity, a targeted treatment plan was devised, offering the patient much-needed relief. This instance highlights how MINIP can be a game-changer in pulmonary diagnostics, ensuring that even air-filled structures are meticulously examined.
Orthopädie Rosenberg, a leading orthopedic practice, often dealt with complex cases requiring intricate surgeries. In one such case, a patient with a complicated bone fracture presented a surgical challenge. Traditional imaging provided a limited perspective, making surgical planning difficult.
Turning to 3D rendering, orthopedic surgeons could visualize the fracture in three dimensions, rotating and analyzing it from various angles. This comprehensive view allowed for meticulous surgical planning, ensuring precision during the procedure.
Post-surgery, the same 3D images were used to educate the patient about the fracture and the surgical intervention, fostering understanding and trust. This case exemplifies the multifaceted benefits of 3D rendering in orthopedics, from surgical planning to patient education.
The medical imaging world has evolved regarding diagnostic tools and how these images are stored and accessed. Traditionally, medical images were stored on-premise, requiring significant infrastructure and often leading to challenges in accessibility and sharing.
The shift to cloud-based PACS (Picture Archiving and Communication Systems) marked a transformative phase in medical imaging. With images stored on secure cloud servers, healthcare professionals could access them from anywhere, anytime, ensuring that physical constraints did not bind diagnostics.
Imagine a scenario where a radiologist in New York needs to consult with a neurologist in London. With traditional systems, sharing medical images would involve cumbersome processes, often leading to delays. However, with cloud-based PACS, this sharing becomes instantaneous.
Platforms like PostDICOM allow seamless access to medical images, irrespective of geographical boundaries. This facilitates collaboration among healthcare professionals and ensures that patients receive timely and informed care, regardless of where they or their doctors are.
The true power of cloud-based PACS is realized when integrated with advanced image processing tools. Tools like MPR, MIP, and 3D rendering offer an unparalleled diagnostic experience when available on cloud platforms.
Healthcare professionals can manipulate and analyze images using advanced tools, all while benefiting from the convenience and accessibility of the cloud. This integration ensures that advanced diagnostics are not restricted to high-end medical facilities but are accessible to clinics and practices of all sizes, democratizing quality healthcare.
One of the primary concerns with cloud storage is security. Patient medical images contain sensitive information, and ensuring their confidentiality is paramount. Cloud-based PACS providers, like PostDICOM, prioritize security, implementing state-of-the-art encryption and compliance measures.
Regular updates, multi-factor authentication, and stringent access controls ensure that medical images are not only easily accessible but also protected from potential breaches. This commitment to security fosters trust among healthcare professionals and patients alike, ensuring that the shift to the cloud is not just about convenience but also about uncompromised safety.
 - Created by PostDICOM.jpg)
The rise of telemedicine has been one of the most significant healthcare trends in recent years. With the ability to consult, diagnose, and even treat patients remotely, geographical boundaries that once posed challenges are now becoming obsolete. However, the success of telemedicine hinges on the quality of diagnostics.
It's one thing to consult a patient via video, but how do you ensure that the diagnostic process is as robust as an in-person visit?
This is where advanced image processing tools come into play. With tools like MPR, MIP, and 3D rendering, healthcare professionals can delve deep into medical images, extracting crucial insights for accurate diagnosis. For instance, a neurologist sitting miles away can use these tools to analyze a patient's brain scans in detail, ensuring that no anomaly goes unnoticed.
These tools enhance the diagnostic accuracy of telemedicine consultations and instill confidence in patients, assuring them that they are receiving top-notch care, irrespective of distance.
One of the standout features of integrating advanced imaging tools with telemedicine is the ability for real-time collaboration. Consider a scenario where a general practitioner, during a remote consultation, comes across a concerning anomaly in a patient's X-ray.
With advanced tools, they can instantly collaborate with a specialist, sharing the image, using tools like 3D rendering for a comprehensive view, and jointly diagnosing the issue. This collaborative approach ensures that patients benefit from multi-disciplinary expertise without needing multiple appointments or travel.
Telemedicine and advanced imaging tools also play a pivotal role in patient empowerment. Patients can access their medical images, use tools to understand their conditions better, and actively participate in their healthcare decisions.
This democratization of healthcare, where patients are not just passive recipients but active participants, is reshaping the doctor-patient dynamic, fostering trust, understanding, and better health outcomes.
Medical imaging has witnessed a paradigm shift, transitioning from basic visualizations to intricate, detailed insights thanks to advanced image processing tools.
As we've journeyed through their evolution, applications, and integration with cloud-based PACS, it's evident that these tools are not just technological marvels but catalysts for transformative patient care.
Their role in telemedicine further underscores their significance in a world where healthcare is becoming increasingly digital and borderless.
As we look to the future, the fusion of these advanced tools with platforms like PostDICOM promises a healthcare landscape where diagnostics are precise, accessible, and patient-centric, heralding a new era of medical excellence.
|
Cloud PACS and Online DICOM ViewerUpload DICOM images and clinical documents to PostDICOM servers. Store, view, collaborate, and share your medical imaging files. |